Periodontal disease is a disease of the gums and bone which support the teeth. It affects, to one degree or another, a vast majority of the adult population in the United States. The beginning of the disease manifests itself as an inflammation of the gums known as gingivitis. If left untreated, the disease may progress to periodontitis, which in its early stages will effect the bone levels around existing teeth. As the disease progresses more and more bone is lost. In advanced periodontitis, tooth loss is the inevitable outcome. The disease process is due to a bacterial infection of the gums and the bone that supports the teeth.
The bacteria colonize in the gingival tissue. This bacterial colonization will lead to gingival inflammation, causing a pocket to form between the teeth and the gums. If these bacterial colonies are removed promptly, in the early stage of the disease process known as gingivitis, the effects of the disease are completely reversible. If these bacterial colonies are left untreated, however, the disease process will spread to the underlying bone and will begin to destroy it. As teeth lose their supporting bone, they will get loose and may eventually be lost.
While intraoral environmental factors play the major role in the development of periodontal disease, studies have shown familial tendency to develop the disease. The best way to prevent the disease, however, is through the use of easy preventative measures, which if adhered to, may in most cases prevent the onset of the disease process completely.
Here are some of the most common causes of gum disease:
Poor oral hygiene:
Good oral home care, including proper brushing and flossing, a healthy diet and regular dental visits are the best way to maintain good oral hygiene and prevent the build up of plaque and calculus. In the absence of good oral hygiene, plaque and calculus will accumulate on the teeth and will effect the gum and the supporting bone structure leading to gingivitis and periodontitis.
Tobacco use:
Among the most significant causes of periodontal disease is tobacco use. Smokers are far more likely to develop periodontal disease, will build up plaque at a faster pace and are less likely to respond positively to periodontal treatments than are non-smokers.
Genetic or familial predisposition:
Studies have shown that nearly 30% of the population has either a familial or genetic predisposition to periodontal disease. These patients will be six times more likely to suffer the consequences of periodontal problems than the general population. Even with outstanding oral home care, these patients tend to develop the symptoms of the disease. It is imperative that this segment of the population be seen by a periodontist on a regular basis to assess the development and progress of periodontal disease.
Pregnancy and menopause:
Pregnancy and the hormonal changes associated with it tend to lead to the development of gingivitis. It is imperative to have a meticulous oral hygiene regimen during pregnancy.
Chronic stress and poor diet:
Poor diet and a high level of stress tend to lower the body’s ability to fight off infection and weaken the immune system in general. These contributing factors will effect oral health to a great degree. People undergoing high stress thresholds who have poor diets are much more likely to develop periodontal disease.
Diabetes and underlying medical issues:
Many medical conditions can exacerbate the onset and progression of periodontal problems. These include, but are not limited to, diabetes, heart disease, circulatory problems and osteoporosis.
Malocclusion and oral habits:
Harmful oral habits such as grinding or clenching of the teeth are also contributing factors to periodontal disease. Malocclusion, the lack of a proper bite, also may promote and exaggerate the effect of the disease process.
Medication:
Many medicatons have oral manifestations which may lead to periodontal problems. Many of these medications inhibit salivary flow which also promotes periodontal disease.
Periodontal disease manifests itself in many different ways, all of which require early intervention by a periodontist and other oral healthcare professionals. Early treatment will result in much better prognoses and treatment outcomes.
Gingivitis is the mildest and most common form of periodontal disease. It is characterized by gum inflammation without involvement of the supporting bone structures of the teeth. If treated at an early stage, gingivitis is totally reversible.
Gingivitis is treated by a combination of meticulous home care and professional cleaning. The dentist may perform root planing and deep scaling procedures to remove the plaque and calculus which are the causative factors of the inflammation.
Chronic periodontal disease, while it may effect younger people, occurs much more frequently in people over 40. Chronic periodontal disease is characterized by gingival inflammation and bone loss. Once bone is lost, it cannot be restored. Chronic periodontitis is not reversible.
The goal in treating chronic periodontitis is to halt the progression of the disease. This is accomplished using several different regimens. The first is the reinforcement of the patient’s oral hygiene and home care. The periodontist will then remove the plaque and calculus that are causing the disease process to progress by using scaling and root planing procedures in combination with debriding the infected material that line the pocket formed between the teeth and the gums. The periodontist may also treat the pockets with antimicrobial agents. The periodontist may also perform surgical treatments such as pocket reduction surgery and tissue grafts to strengthen the bone and improve the aesthetic appearance of the oral cavity. In some cases, dental lasers may be used to treat the pockets and halt the progress of the disease.
Many systemic illnesses may cause or worsen the effects of periodontal disease. Among the most common of these are heart disease, diabetes and respiratory disease. In these cases, the patient may have aggressive periodontal disease even though they maintain excellent oral hygiene and little plaque and calculus is evident.
Initially, the medical condition which caused the onset of periodontal disease must be controlled. The periodontist can then treat the disease using all of the treatment possibilities mentioned above.
While rare, this form of periodontal disease is very aggressive. It generally effects people who suffer from HIV, immunosuppression, malnutrition, chronic stress or smokers. This aggressive form of the disease causes rapid bone loss and tissue necrosis (destruction).
Because it may be associated with HIV or another serious medical condition, the periodontist will work hand-in-hand with the treating physician to develop a treatment plan. Scaling, root planing, antibiotics, medicated mouth rinses and fungicidal medicines are all used to treat this form of the disease.
While the main goal of periodontal therapy is to preserve the health of the supporting structures of the teeth, there are several procedures that we perform to enhance dental aesthetics and improve the look of a patient’s smile. For patients presenting with gum recession or a “toothy” smile, gum grafting procedures may be performed to cover the areas of recession. For patients with a “gummy” smile or teeth that appear to be short, crown lengthening procedures are a relatively simple answer to solve this aesthetic problem.
Periodontal disease is caused by the buildup of plaque and calculus around the gum line and between the teeth. In order to prevent disease, it is imperative to remove these etiologic agents. This will prevent bacterial growth which leads to bone breakdown and advancement of the disease process. The objective of scaling and root planning is to physically remove the plaque and calculus which causes the disease. Scaling and root planning is a non-surgical procedure which is particularly effective in dealing with gingivitis and early stages of periodontitis. If performed effectively at these stages, no further periodontal treatment may be necessary.
After conducting a thorough examination of the oral tissues and viewing radiographic findings, we may suggest scaling and root planning treatments. Depending on the severity of the disease process and the amount of plaque and calculus, local anesthesia may be used to make the treatment more comfortable.
Scaling involves the removing of debris from the crown and root surfaces. This may be accomplished with the use of a combination of ultrasonic and hand scalers. After all the plaque and calculus are “scaled” away, root planning may be undertaken using hand instruments to smooth the root surfaces of the tooth. Smooth root surfaces help prevent the buildup of the agents which cause periodontal disease.
After scaling and root planning procedures eliminate the causative factors, the remaining pockets may be treated with antibiotics.
Periodontal disease is caused by bacterial growth. This bacteria breaks down the periodontal lining of the gum and as the disease progresses, bacteria will begin to break down the supporting tooth structure which surrounds the teeth. One of the most effective ways to kill bacteria is to introduce antibiotics. These antibiotics may be prescribed orally, in pill form, or may be applied locally directly to the areas of the mouth that are periodontally infected.
Over the past several years, direct application of antibiotic into the periodontal pocket has proven to be very effective in halting the disease process if done in combination with other periodontal procedures.
Systemic antibiotics can be prescribed at a low dose for long term periodontal use, or as a short term medication to treat acute periodontal infections.
Oral and Locally Delivered Antibiotics
Several different antibiotics have proven to be useful and particularly effective in the treatment of periodontal disease.
Tetracycline antibiotics: The tetracycline family of antibiotics, which include tetracycline hydrochloride, doxycycline, and minocycline are generally thought of as the primary drugs used in periodontal treatment.
Macrolide antibiotics: Known for their effectiveness in reducing gingival inflammation, this family of antibiotic is often used for patients suffering from periodontitis.
Metronidazole: This antibiotic is generally used in combination with amoxicillin or tetracycline to combat inflammation and bacterial growth in severe or chronic periodontitis.
Arestin®: This antibiotic, which is delivered right into the gingival sulcus (pocket within the gum) has proven very effective in slowing the disease process and inhibiting bacterial growth.
Periodontal disease is caused by bacteria which infect the periodontal lining of the gum. If not removed, this bacterial growth will spread and will begin to destroy the bone that supports the teeth. As bone is destroyed by the bacteria that is found on plaque and calculus, pockets form between the teeth and gums. As these pockets become deeper, it is almost impossible to clean the bottom of the pockets using toothbrushing and flossing techniques. If the pockets are not adequately cleaned and debrided, they will continue to deepen and more bone will be destroyed. This destructive cycle will continue and will eventually lead to tooth loss. The goal of all periodontal surgical procedures is to eliminate the pocket and to allow the patient to keep the gums and teeth clean using proper brushing and flossing techniques.
hile a surgical procedure, periodontal surgery is generally very well tolerated by patients and in most cases can be performed under local anesthesia.
An incision will be made to allow us to gently pull the gum tissue away from the teeth. All calculus and plaque will be meticulously removed and all root surfaces will be smoothed. Antibiotic may be placed in the surgical site. The gum tissue will then be sutured back into place eliminating the pocket. In many cases a protective packing may be placed to keep the area clean and to facilitate faster healing.
The suture material (stitches) generally will remain in the mouth for 7-10 days.
Though the gums will be more sensitive immediately following the procedure, there will be a significant reduction in pocket depth and a vast improvement in the condition of the teeth and gums.
Periodontics can often be used to make your front teeth look better
Gingival recession is a problem which effects millions of Americans. It may be caused by toothbrush abrasion, periodontal disease or simply as a product of aging. When gingival recession occurs the teeth appear longer, the root surface is exposed and generalized sensitivity of the teeth occurs. These problems can all be addressed by the use of gingival grafting. This is a procedure where we can literally move the gum to a position that covers more of the tooth structure. This can also be accomplished by using graft tissue – either an autograft from the patient’s palate or a synthetic graft to cover the exposed tooth surfaces. Any type of this procedure will alleviate the sensitivity and will allow for an outstanding aesthetic result.
In order to begin treatment, it is essential to do a thorough, complete and extensive examination. We will review the patient’s medical history to determine if there are any factors that may influence the development of periodontal disease or limit the scope of treatment. Additional x-rays may be taken as a further diagnostic tool. An oral cancer screening will also be performed during your initial visit to our office.
A periodontal charting of the entire dentition with measurement and recording of several key parameters for each tooth will be completed. We will then be able to assess the degree and severity of the periodontal disease present. A comprehensive periodontal evaluation typically includes gently measuring the depth of the pocket between the tooth and gum with a periodontal probe. One measurement is recorded for each of six zones on each and every accessible tooth. Any gum recession or tooth mobility will also be charted and evaluated at this stage.
For those patients interested in dental implants, we may suggest that a 3 dimensional CBCT dental scan be taken. This will allow us to assess the thickness and height of the jaw bone to evaluate the proper placement of the dental implant.
An accurate diagnosis is the foundation upon which all of your treatment recommendations are made. Whether the patient is seeing us for a full mouth rehabilitation or a single tooth procedure, the correct diagnosis is the key to any and all treatment planning.
Gum disease begins when a film called plaque accumulates on the teeth. Certain strains of bacteria that live in this plaque damage gum tissue and bone. Your body tries to fight this infection with an inflammatory assault, sending white blood cells to the area to destroy the bacteria. This inflammation causes the tissue to bleed easily when you brush or floss. This stage of the condition is called gingivitis.
If the infection and inflammation persist, what results is a chronic inflammatory condition in which the gums and bone around the teeth are slowly destroyed, many times with no awareness or symptoms. At this stage, it is called periodontitis.
The biggest risk factors are ineffective home care, poor nutrition, and smoking. Periodontitis has been linked to an increased risk of heart disease, diabetes, stroke, and other serious medical conditions. In short, healthy gums are the gateway to a healthier body.
Gingivitis can be reversed with regular professional cleanings and excellent home care. It is also important to eat healthy foods such as fresh fruits and vegetables. These types of foods have important anti-oxidants and phytonutrients your body needs to remain healthy.
Once your condition has progressed to periodontitis, surgical intervention is often necessary to eliminate the deep pockets which develop between the teeth and gums. If these pockets persist, they allow bacteria to organize even more colonies and this often leads to tooth loss.
Traditional gum surgery involves cutting away some of the gum tissue, and reshaping the bone underneath. LANAP is a less invasive technique using a specialized laser to destroy the bacteria which caused the disease, and alter the tissue so that it has the opportunity to heal. The use of laser preserves more tissue than traditional scalpel surgery, and results in a faster and less painful recovery.
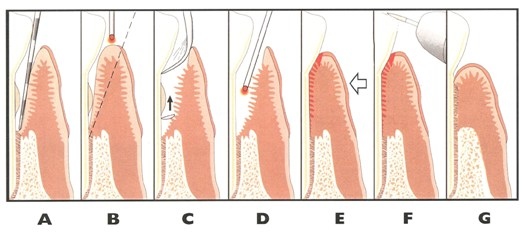
A. Depth of pocket is measured under anesthesia
B. Laser selectively removes infected pocket lining
C. Ultrasonic instruments clean root surfaces
D. Laser disinfects pocket and creates blood clot
E. Tissue is compressed against the tooth
F. Bite is adjusted through selective grinding
G. Healing results in new attachment after 12 months
Usually, we treat one half of the mouth at a time. The surgical visits are ideally made one to two weeks apart, and take about two to three hours each on average.
The mouth is numbed, just like if you were having a filling or crown done. Sedation is available if you prefer. The pockets are then measured while you are numb, so that more accurate measurements can be made without causing discomfort.
A first pass is made with the laser, removing the infected pocket lining and allowing better visualization of the roots of the teeth. Then the teeth are cleaned very thoroughly using ultrasonic instruments, which have tips that vibrate very quickly, loosening up any deposits on the teeth and flushing them away with an irrigating solution.
A second pass is made with the laser, disinfecting the pockets and sealing them up through the formation of a stable blood clot. The bite is then adjusted to minimize destructive, uneven biting forces on the teeth.
Most people experience some mild soreness of the treated areas for the first few days. The tissue will appear discolored around the teeth, similar to what a scab looks like when you get it wet. It is very important NOT to brush or pick this away, as this fibrin barrier is what allows the gums underneath to get a head start creating a new attachment to the teeth.
Your bite will feel different, as if the teeth don’t touch together as heavily on the treated side. This can feel imbalanced at first, but the teeth will quickly adapt. After both sides have been treated, and as further refinements are made, your bite should feel stronger and more stable than ever, and more comfortable.
As the gums heal, the teeth will shift, and your bite will need to be adjusted several times over the first few weeks, even for the first year and beyond. Although it seems counter-intuitive, inadequate adjustment is what is usually responsible for soreness or sensitivity following LANAP.
Three to six weeks after your surgery, impressions will be made of your teeth, and a bite guard will be fabricated to stabilize and immobilize the teeth while you sleep. It is important to wear these night splints, as we humans have the tendency to periodically clench our teeth and jaws during sleep. This clenching can produce extremely damaging forces which can delay or prevent healing.
Professional cleaning is recommended every three months for the first year, and re-evaluation of your condition will be done after the twelve month visit. Most people with gum disease remain at risk for the rest of their lives, and would benefit from having their teeth cleaned every three months indefinitely.
-LANAP (one side of mouth)
Prescriptions for swelling and pain
NO BRUSHING!
NO FLOSSING!
NO SMOKING!
-LANAP (other side of mouth)
Same as above
-1 Week post-op visit
Splint loose teeth together
Bite adjustment
Begin modified brushing
NO flossing or electric toothbrush
-1 Month post-op visit
Light cleaning/polishing of teeth
Bite adjustment
Resume brushing and flossing
Impressions for biteguard
-2 Month post-op visit
Light cleaning/polishing of teeth
Bite adjument
Deliver biteguard (wear every night)
-3 Month maintenance visit
-6 Month maintenance visit
-9 Month maintenance visit
-12 Month maintenance visit
-1 Year re-evaluation
Full periodontal charting, x-rays
Assess need to retreat any persistent or non-responsive areas
Discuss direction of future treatment
Including any recommended restorative, cosmetic, or orthodontic care
The cost of laser surgery is generally slightly more than traditional surgery, and will depend upon the severity and complexity of your condition. At your initial consultation, we can identify your specific situation, and give you an estimate of what your cost would be.
For further information about the LANAP Protocol, Visit www.millenniumdental.com.
Oral cancer includes cancers of the mouth and the pharynx (the back of the throat). Oral cancer accounts for roughly two percent of all cancers diagnosed annually in the United States. Approximately 35,000 people will be diagnosed with oral cancer each year and about 7,600 will die from the disease. On average, 60 percent of those with the disease will survive more than 5 years. Oral cancer most often occurs in people over the age of 40 and affects more than twice as many men as women.
Tobacco and alcohol use. Most cases of oral cancer are linked to cigarette smoking, heavy alcohol use, or the use of both tobacco and alcohol together. Using tobacco plus alcohol poses a much greater risk than using either substance alone.
HPV Infection with the sexually transmitted human papillomavirus (specifically the HPV 16 type) has been linked to a subset of oral cancers.
Age. Risk increases with age. Oral cancer most often occurs in people over the age of 40.
Sun Exposure. Cancer of the lip can be caused by sun exposure.
Diet. A diet low in fruits and vegetables may play a role in oral cancer development.
See a dentist or physician if any of the following symptoms lasts for more than 2 weeks.
It is important to find oral cancer as early as possible when it can be treated more successfully. An oral cancer examination can detect early signs of cancer. The exam is painless and takes only a few minutes. Your regular dental check-up is an excellent opportunity to have the exam. During the exam, your dentist or dental hygienist will check your face, neck, lips, and entire mouth for signs of cancer.
Periodontal disease is caused by the buildup of plaque and calculus around the gum line and between the teeth. In order to prevent disease, it is imperative to remove these etiologic agents. This will prevent bacterial growth which leads to bone breakdown and advancement of the disease process. The objective of scaling and root planning is to physically remove the plaque and calculus which causes the disease. Scaling and root planning is a non-surgical procedure which is particularly effective in dealing with gingivitis and early stages of periodontitis. If performed effectively at these stages, no further periodontal treatment may be necessary.
After conducting a thorough examination of the oral tissues and viewing radiographic findings, we may suggest scaling and root planning treatments. Depending on the severity of the disease process and the amount of plaque and calculus, local anesthesia may be used to make the treatment more comfortable.
Scaling involves the removing of debris from the crown and root surfaces. This may be accomplished with the use of a combination of ultrasonic and hand scalers. After all the plaque and calculus are “scaled” away, root planning may be undertaken using hand instruments to smooth the root surfaces of the tooth. Smooth root surfaces help prevent the buildup of the agents which cause periodontal disease.
After scaling and root planning procedures eliminate the causative factors, the remaining pockets may be treated with antibiotics.
The bone that surrounds the roots of the teeth is referred to as the alveolar ridge. A ridge augmentation is a surgical procedure performed to restore the normal height and width of the alveolar ridge that may have been diminished as a consequence of having a tooth removed or for other reasons like denture wear or trauma. The main considerations when a reduced and narrowed alveolar ridge is present are how this lost tissue will effect the placement of a dental implant or other dental prosthesis.
A ridge augmentation procedure is performed by placing bone graft material into the tooth socket or immediately after a tooth has been removed or where there are deficient areas in order to rebuild the shape of the gums and jaw. While in certain situations dental implants can be placed at the time of a ridge augmentation procedure, they are more often placed after sufficient healing has occurred during which time the bone graft has successfully fused with the existing bone and new bone has formed. Bone graft materials can be collected from another area of the body, harvested from other natural sources, or can be made of synthetic materials. The choice depends upon the specific needs of the case.
When replacing posterior upper teeth with dental implants, one of the limiting factors is the amount of bone available between the gum and the maxillary sinus. If there is insufficient bone to allow for the placement of an implant, we may suggest a procedure called a sinus augmentation procedure or a sinus lift. During this procedure, the sinus membrane is then lifted upward and donor bone is inserted into the floor of the sinus. After several months of healing, the bone becomes part of the patient’s jaw and dental implants can be inserted and stabilized in this new sinus bone. Routine dental implant procedures can then be performed.
Periodontal disease is caused by bacteria which infect the periodontal lining of the gum. If not removed, this bacterial growth will spread and will begin to destroy the bone that supports the teeth. As bone is destroyed by the bacteria that is found on plaque and calculus, pockets form between the teeth and gums. As these pockets become deeper, it is almost impossible to clean the bottom of the pockets using toothbrushing and flossing techniques. If the pockets are not adequately cleaned and debrided, they will continue to deepen and more bone will be destroyed. This destructive cycle will continue and will eventually lead to tooth loss. The goal of all periodontal surgical procedures is to eliminate the pocket and to allow the patient to keep the gums and teeth clean using proper brushing and flossing techniques.
While a surgical procedure, periodontal surgery is generally very well tolerated by patients and in most cases can be performed under local anesthesia.
An incision will be made to allow us to gently pull the gum tissue away from the teeth. All calculus and plaque will be meticulously removed and all root surfaces will be smoothed. Antibiotic may be placed in the surgical site. The gum tissue will then be sutured back into place eliminating the pocket. In many cases a protective packing may be placed to keep the area clean and to facilitate faster healing.
The suture material (stitches) generally will remain in the mouth for 7-10 days.
Though the gums will be more sensitive immediately following the procedure, there will be a significant reduction in pocket depth and a vast improvement in the condition of the teeth and gums.
While the goal of periodontal procedures are to eliminate pocketing and maintain bone support, some periodontal procedures are indicated to improve esthetics or to allow for the maintenance of a severely broken down tooth. One such procedure is periodontal crown lengthening.
This procedure is indicated in the case of a “gummy” smile where the teeth have adequate length but are covered by too much gum tissue. During this procedure, excess gum and bone tissue is reshaped to expose more of the natural tooth. This can be done to one tooth, to even your gum line, or to several teeth to expose a natural smile.
Your dentist may also recommend crown lengthening for restorative reasons. If a tooth is too short to restore or is broken down below the gum line, we can perform a crown lengthening procedure to expose more tooth structure to allow your dentist to save the tooth and to place a long lasting restoration.
Gum recession causes root exposure. This poses two problems. One is an esthetic problem causing the teeth to appear longer. Exposed root surfaces also cause tooth sensitivity.
In order to cover these exposed roots, we can perform soft tissue graft procedures.
During this procedure, we will remove gum tissue from your palate or another donor source to cover the exposed root. This can be done for one tooth or several teeth to even your gum line and reduce sensitivity.
When a tooth is extracted, the bone where the tooth once was will resorb over a period of time. This may leave a situation where the bone is too narrow or insufficient to accept a dental implant.
Bone grafting procedures will allow for adequate bone height and width to accept dental implants. Using bone grafting procedures, we can actually stimulate bone growth in areas where bone is insufficient.
Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease or injuries. The bone is generally obtained from outside sources but may sometimes also be taken from the patient’s own bone.
Once bone growth is stimulated and bone height and width are adequate, implant placement is possible.
Guided bone regeneration is a dental procedure that is used for increasing bone mass in cases where vertical and/or horizontal defects in the jawbone exist. It is a reliable method for re-establishing hard tissue volume in areas of bone loss, which has taken place in the upper or lower jaw as the result of periodontal disease, trauma, cyst or tumor surgery, or subsequent to a dental extraction.
During a guided bone regeneration procedure a special membrane is positioned to cover a newly placed bone graft in the area of a bony defect. This membrane facilitates new growth of bone, while preventing any growth of unwanted soft tissue into the area.
Guided bone regeneration can enable the placement of dental implants in cases in which implants would otherwise not be possible.
To preserve dental health as well as overall well being, it is sometimes necessary to have a tooth extracted. In many cases a tooth extraction is the result of dental disease or injury. However, without teeth in place the soft tissue and the supporting bone in the area may degenerate or shrink. This can complicate future efforts to fabricate a replacement tooth like a dental bridge or dental implant.
Ridge preservation is a procedure designed to retain the soft tissue and bone structure at the site of an extracted tooth. After a tooth is removed bone-grafting material is placed in the socket to promote healing and encourage new bone development. Maintaining adequate bone and supporting the soft tissues following a tooth extraction by means of a ridge preservation procedure, facilitates the successful placement of a dental implant.
An impacted tooth is one that fails to erupt and remains covered to varying degrees by the soft tissue and bone. After the wisdom teeth, the most frequently impacted teeth are the maxillary canines. Since the canines play such an important role in the dental arch in terms of optimal function and facial support, it is important whenever possible to bring these teeth into alignment.
In situations involving an impacted canine, an orthodontist will develop a treatment plan. This is typically followed by the placement of orthodontic appliances and the development of space as needed for the impacted tooth. At the appropriate juncture in treatment, the patient is referred for a surgical procedure to remove the necessary amount of bone and soft tissue covering the canine. During this surgical procedure an orthodontic attachment to facilitate moving the tooth into alignment will be placed on the tooth. Once sufficient healing has taken place, the orthodontist can proceed to gradually move the canine into its proper position.
A frenum (also known as a frenulum) in the oral cavity is a fold of tissue connecting moveable soft tissue such as the lips, cheeks or tongue to the fixed tissues next to the teeth and floor of the mouth. This fold of tissue can contain some muscle fibers as well.
The major frena in the mouth can be seen in three locations. The first is the maxillary labial frenum located on the underside of the middle of the upper lip connecting it to the gum tissue above and between the front two teeth on top. Another frenum is the mandibular labial frenum on underside of the lower lip connecting it to the gum tissue below and between the front two teeth on bottom. The third is the lingual frenum is on the underside of the tongue connecting it to the floor of the mouth.
In most cases these frena do not adversely limit tongue function or affect the teeth or their surrounding hard and soft tissues. However, there are situations where they do and a surgical procedure is required. A maxillary labial frenectomy is the most common one performed, and is considered when a large and ropey frenum is attached too close to the crowns of the teeth or extends too far towards the roof of the mouth. This causes space between the two front teeth, keeps the teeth apart, and can even affect the gums and bone between the front two teeth. A lingual frenectomy is considered when the lingual frenum attaches too far forward on the tongue and is impairing function including, speech, swallowing or eating.
When an abnormal frenal attachment is present certain surgical procedures like a frenectomy to remove a portion of the frenum can be performed. This prevents further tissue damage, allows for appropriate tooth movement and stability, and restores normal function.
Every time that you close your mouth or bite down or bring your teeth together there should be a healthy distribution of forces. Furthermore, the top teeth should appropriately contact the bottom teeth during jaw movement in a functionally harmonious way. Having premature or uneven contact between the upper and lower teeth can lead you to experience unhealthy jaw deviations when biting as well as other symptoms of soreness or discomfort.
An occlusal adjustment is a procedure to correct uneven contacts or bite interferences to restore the healthy distribution of forces to your teeth as they function. It involves the selective minor filing and reshaping of the occlusal or incisal surfaces (biting surfaces) of the teeth. An occlusal adjustment is a precise procedure that in most cases creates no discomfort. The adjustment may be performed on a single tooth, or on multiple teeth as needed.
Today, with advanced dental technology even the slightest bite discrepancies can be detected, allowing you to receive the most precise occlusal adjustments.
Periodontal splinting is a procedure whereby teeth that are mobile are connected to each other to improve their stability and comfort during jaw closure, biting, and chewing. By splinting teeth that have weakened support, the prognosis for maintaining these teeth in the mouth is better. The added stability provided by periodontal splinting also promotes optimal results with tissue regeneration procedures.
Cases that may require periodontal splinting include, teeth whose support has been compromised by periodontal disease or trauma. When multiple teeth are splinted together the biting force can be sustained by the entire joined unit, rather than the individual teeth. Periodontal splints can be fabricated in a number of ways including placing composite resin to secure a section of a reinforced ribbon applied to the involved teeth.
In cases of periodontal disease, an osseous grafting procedure may be necessary to address the bony defects caused around a tooth by the progression of periodontal disease. An osseous grafting procedure, which involves guided tissue regeneration, rebuilds the bone and supporting tissues that have been lost. During the surgical procedure the roots of the involved teeth are thoroughly cleaned and the bony defects prepared and filled with a suitable bone graft material. The bone graft is then covered by a special membrane and then the gums are sutured back into place. With healing and time the osseous graft will fill in for the lost bone, thereby providing renewed support for the tooth.
By the age of eighteen, the average adult has 32 teeth; 16 teeth on the top and 16 teeth on the bottom. Each tooth in the mouth has a specific name and function. The teeth in the front of the mouth (incisors, canine and bicuspid teeth) are ideal for grasping and biting food into smaller pieces. The back teeth or molar teeth are used to grind food up into a consistency suitable for swallowing.
The average mouth is made to hold only 28 teeth. It can be painful when 32 teeth try to fit in a mouth that holds only 28 teeth. These four other teeth are your Third Molars, also known as "wisdom teeth."
Wisdom teeth are the last teeth to erupt within the mouth. When they align properly and gum tissue is healthy, wisdom teeth do not have to be removed. Unfortunately, this does not generally happen, as wisdom teeth are the most commonly impacted teeth in the mouth. They may grow sideways, partially emerge from the gum and even remain trapped beneath the gum and bone. Impacted teeth can take many positions in the bone as they attempt to find a pathway that will allow them to erupt successfully. The location and impaction of the wisdom teeth can often create periodontal problems associated with teeth in front of them.
These poorly positioned impacted teeth can cause many problems. When they are partially erupted, the opening around the tooth allows bacteria to grow and can cause an infection. The result: swelling, stiffness, pain and illness. The location and impaction of the wisdom teeth can also often create periodontal problems with the teeth in front of them. The most serious problem occurs when tumors or cysts form around the impacted wisdom tooth, resulting in the destruction of the jawbone and healthy teeth. Removal of the offending impacted tooth or teeth usually resolves these problems. Early removal is recommended to avoid such future problems and to decrease the surgical risk involved with the procedure.
With an oral examination and x-rays of the mouth, your oral surgeon can evaluate the position of the wisdom teeth and predict if there may be present or future problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid- teenage years by their dentist, orthodontist or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Your oral surgeon has the training, license and experience to provide various types of anesthesia for patients to select the best alternative.
The removal of wisdom teeth can be performed in the office under local anesthesia, nitrous oxide analgesia (laughing gas) or IV sedation. These options as well as the surgical risks will be discussed with you before the procedure is performed. Once the teeth are removed, the gum is sutured. To help control bleeding, bite down on the gauze placed in your mouth. You will rest under our supervision in the office until you are ready to be taken home. Upon discharge, your post-operative kit will include postoperative instructions, a prescription for pain medication, antibiotics and a follow-up appointment in one week for suture removal. If you have any questions, please do not hesitate to call us.
Sometimes it is necessary to extract a tooth. This can happen for a variety of reasons. Extractions are commonly performed in cases where a deciduous “baby” tooth is reluctant to fall out, a severely broken down and non-restorable tooth is present, or “wisdom tooth” is poorly positioned and unable to fully erupt into place.
To reduce any anxiety and insure patient comfort whenever a tooth extraction is necessary, the procedure, the post surgical instructions, as well as any restorative follow-up care will be carefully and completely explained.
The oral and maxillofacial region consists of hard and soft tissues that have many different and important functions. Oral pathology refers to the wide range of diseases and conditions manifesting themselves and affecting this area of the body. The signs and symptoms of these problems might be localized and have minor implications for an individual’s overall health, or may be a sign of larger systemic (throughout the body) medical conditions. However, suspicious lesions in the mouth and maxillofacial region can also be cancerous and can lead to far more serious consequences if not detected and treated promptly.
If tissue abnormalities or lesions are present in the oral and maxillofacial area it must be determined if they are the result of congenital or genetic conditions, infection, trauma, environmental causes, have developed for another medical reason or are idiopathic (without a known cause). A patient’s medical history, including lifestyle and habits in conjunction with a description of any signs and symptoms that a patient is experiencing can provide helpful information towards a diagnosis. Following a clinical exam, a biopsy as well as further diagnostic testing, is performed as needed to identify the source of the pathology.
If an individual on their own notices any suspicious growths, ulcerations, or unusual bumps anywhere in their mouth or in the head and neck region, it is important that they have them promptly evaluated.
As the result of a dental injury a tooth can be partially pushed into its socket. When this happens immediate dental care is required to reposition and stabilize the tooth. If a permanent tooth has been dislodged, a root canal treatment is usually needed and should be initiated within a few days of the injury. As part of the treatment a special medication called Calcium Hydroxide is placed inside of the tooth.
In situations where a tooth is partially pushed out of its socket, immediate dental care to reposition and stabilize the tooth is also required. If the pulp of the tooth remains healthy, no other treatment is necessary. However, if the pulp becomes damaged or infected, a root canal therapy is necessary.
When a tooth has been completely knocked out of the mouth, it is important to get to the endodontist as quickly as possible. It is important to handle the tooth carefully to avoid further damage. The main thing is to keep the tooth moist. You can place the tooth in milk or a glass of water (add a pinch of salt). Saving the tooth in large part depends upon the length of time the tooth was out of the mouth and the way the tooth was handled and stored. Keep in mind that only permanent teeth should be re-implanted.
Chronic jaw clenching and grinding one’s teeth is called bruxism. While it can happen any time of day, it often occurs at night causing an individual to wake up with any number of symptoms including jaw pain, headaches, and sore teeth that may feel loose. Although, stress and anxiety are the most common causes of bruxism there may be other contributing factors such as a sleep disorder, an abnormal bite, as well as teeth that are missing or poorly aligned.
To alleviate the symptoms of bruxism, wearing a night guard while sleeping is frequently recommended. This appliance is designed to fit over the teeth and to keep the jaws slightly apart. Wearing a night guard prevents a number of damaging events including muscle strain, excessive pressure on the jaw joint (the TMJ), and such dental damage as chipped or cracked teeth resulting from the teeth grinding against each other.
In addition to preventing damage to the soft and hard tissues surrounding the orofacial cavity, a custom night guard fabricated at the dental office can help curb a bruxism habit and give the wearer a better night’s sleep.
Among the most common, irritating and difficult to diagnose problems with head and neck pain are temporal mandibular joint problems, more commonly known as TMJ problems. The joint is located near the ear where the top of the mandible or lower jaw meets the upper jaw at the base of the skull.
Like all other joints in the body, the TMJ is subject to inflammation and other chronic joint problems. Many of these issues may be caused by destructive bite habits like clenching or grinding. These actions cause pressure on the joint that can lead to inflammation and general breakdown of the joint itself.
What makes TMJ problems difficult to diagnose and treat properly is the fact that the symptoms vary widely in both location and severity. Symptoms can range from a slight clicking in the jaw with no pain to severe head and neck pain which is not relieved by medication.
Once diagnosed properly treatments include everything from simple placement of a nightguard, which prevents pressure on the joint to surgical intervention in more severe cases. A dental health professional is the person most able to diagnose this widely variable and very common issue.
Perhaps the greatest advance in the field of dentistry over the past generation has been the advent of the osteointegrated dental implant. Today’s dental implant can provide a patient with the ability to replace partial and full dentures and to restore missing teeth without the necessity of using other teeth as anchors. Fixed bridgework can replace removable partial dentures and implants also allow for the stabilization of previously loose ill-fitting dentures.
In essence, the implant will replace roots of teeth and will allow the dentist to fabricate restorations over these artificial roots. Dental implants are designed to provide a foundation for replacement teeth that look, feel and function like natural teeth. The person who has lost teeth regains the ability to eat virtually anything and can smile with confidence, knowing that their teeth will appear natural.
In order to determine whether an area where a tooth or teeth are missing would be a good site for a dental implant, it may be necessary to do a full radiographic study of the area including a CBCT 3-dimensional scan. Once a determination that the site is satisfactory to accept an implant is confirmed, a complete treatment plan must be determined by your periodontist and the general dentist or prosthodontist who will be restoring the teeth.
There are many different ways a dental implant and the replacement tooth may be placed. In certain cases, it is possible that a replacement tooth can be placed over an implant in one visit. More frequently, however, placing of a dental implant and restoring a tooth is generally done in several stage.
In stage one of the procedure, we will surgically place the implant body into the jawbone. This is accomplished by making an incision in the gum, preparing the bone to accept the implant and placement of a titanium implant into the bone. The gum is then replaced over the seated implant. The implant is then given time to integrate into the jawbone. Bone will grow around the implant and will provide a solid base for the tooth that is being restored. The length of time allowed for the bone to integrate is very variable. It depends upon the site of the implant, the jaw in which the implant was placed, the density of the existing bone and several other contributing factors. During this time, in many cases, a temporary tooth replacement can be worn over the implant site.
Once the bone has integrated around the implant, we will initiate the next phase of treatment by opening the gum and placing a temporary healing cap into the body of the implant. The patient will then return to the general dentist, where the healing cap will be replaced by a post which will act as the base of a crown. The crown will be created in a laboratory based on an impression made by the dentist. The crown will then be placed and the implant based replacement tooth will be completed. It will function and feel like a tooth and will remain in the mouth permanently. It does not need to be removed.
There are some implant systems (one-stage) that do not require this second step. These systems use an implant which already has the extension piece attached. We will advise you on which system is best for you.
If you are missing a single tooth, one implant and a crown can replace it. A dental implant replaces both the lost natural tooth and its root.
Before dental implants, the only way to restore a missing tooth permanently was to create a fixed bridge. A fixed bridge involved cutting down teeth on either side of the missing tooth and using them as anchors for the bridge. The bridge would then be cemented into the patient’s mouth.
Dental implants offer significant advantages over a fixed bridge:
For hundreds of years, the only way to replace multiple missing teeth has been with removable partial or full dentures. While dentures restore function and are aesthetically satisfactory, they are rarely very comfortable, they do not feel like real teeth and in many cases they are chronically loose. Today the use of multiple dental implants can be used to eliminate dentures completely or to modify them so that they are stable, comfortable functional and aesthetically pleasing.
There are several different treatment options to replace removable or full dentures:
Like individual implants, multiple implants can be placed in the bone to replace all teeth that are missing. Depending on the number of implants and the number of teeth to be replaced, either individual crowns or fixed bridges may be made over the implants. These will be cemented and will remain fixed in a patient’s mouth, virtually replacing all of the teeth that the patient was missing.
For patients with full upper or lower dentures, who either cannot have enough implants placed to allow for fixed bridgework or who do not want to undergo the expense of full arch fixed implants, a new solution is available. The full arch implant prosthesis is a less expensive fixed alternative. Several implants will be placed and either porcelain and acrylic or zirconia teeth in the form of a denture will be fabricated in the lab and placed over the implants. These will be fixed and do not need to be removed. They will provide the patient with a stable fixed solution to replace their existing dentures.
The chronically loose set of dentures can now be replaced by supporting them with multiple dental implants. Dental implants can be placed and either a bar, ball retention or locater will be placed over the implant. The denture will then snap in over the bar, ball or locater locking the denture into place. This will give the patient a denture that is rigid, well functioning and functional. It will eliminate the use of denture adhesives and will allow the patient the ability to eat many of the foods they were unable to with regular dentures.
One of the dental solutions for the treatment of multiple lost or missing is a removable denture. While a removable denture is an effective prosthetic appliance for restoring one’s smile, there can be issues with its stability that affects both comfort and function. However, one way to address this problem is with the placement of mini dental implants.
Mini dental implants are narrower in diameter than traditional dental implants. This makes them an excellent option for providing added denture stability in cases where a grafting procedure to create enough bone would otherwise be needed for the placement of full size implants. Furthermore, mini implants can be placed in a less invasive manner, making them an easier procedure to tolerate for people with certain medical conditions.
An implant-supported denture is fitted with special housings that allow the denture to essentially snap on to the head of the mini implant thereby providing the needed denture stabilization.
The success of a dental implant procedure relies on the establishment of a structural and functional connection between the dental implant and the surrounding jawbone. Osstell technology and systems provide a non-invasive method for assessing the degree of osseointegration and measuring the stability of the dental implant. By providing objective and reliable data on the degree of osseointegration the healing process can be evaluated, thereby making treatment outcomes more predictable.
An advanced information gathering, treatment planning, and computer guided support platform that addresses the initial phases of the implant process all the way through the actual placement of the implants. The Simplant 3D system provides essential analysis and assistance to all facets of the dental implant process from acquiring the diagnostic records to the final restoration procedure. Simplant allows for the most efficient and effective dental implant treatment planning taking into account all of the cosmetic and functional requirements of the patient’s case.
IV Sedation involves a sedative that is administered intravenously, or directly into a vein. It is indicated when deeper sedation is required. This type of sedation can be quickly modified to your state of consciousness and can be continued as long as necessary for the procedure.
Special Instructions: An escort will need to be present for the appointment and be able to drive you home when the appointment is completed. For morning appointments (before 1:00 pm), do not eat or drink after midnight the night before your appointment. For afternoon appointments (after 1:00 pm) with IV sedation, do not eat or drink at least 6 hours prior to your appointment.
Sedation dentistry offers individuals with general anxiety about going to the dentist or fears about a specific dental procedure the opportunity to have a stress free and more comfortable experience. Utilizing safe and controlled sedation techniques prior to the dental procedure the patient is eased into a state of complete relaxation.
Anxiolysis is considered the lightest level of sedation, reducing the stress and anxiety that may be associated with a dental visit or a particular procedure, while an individual maintains their ability to respond appropriately to verbal commands. The usual anxiolysis protocol consists of an oral medication given pre-operatively.
Nitrous oxide or “laughing gas” is inhaled through a small mask over the nose. As the nitrous oxide begins to work, you will feel less nervous. When the procedure is coming to an end the nitrous oxide is turned off, the effects wear off very quickly.
Special Instructions: Individuals slated to have nitrous oxide are advised to eat lightly prior to a procedure. Nausea and vomiting sometimes occur with a full stomach.
Cone-beam computed tomography systems are radiographic systems used by dental professionals to analyze and reconstruct 3D images of a patient’s teeth, jaws and surrounding anatomy. The information obtained by means of CBCT imaging is useful in both diagnosis and precise treatment planning when two-dimensional diagnostic films are insufficient. Dental CBCT is useful for multiple types of analyses as well as the assessment of maxillofacial disorders or pathology. It is also most useful in surgical planning, including the accurate placement of dental implants.
Computer tomography allows us to ensure your implants fit properly. With computer guided surgery, we can virtually complete your procedure before you come in for your scheduled visit. This process will increase the accuracy of the procedure, reduce the length of surgery and improve recovery time.